Sleep problems impact up to 95% of children with autism, often leading to challenges for both the child and their family. When behavioral strategies and sleep hygiene fail, medications may be considered. However, no FDA-approved medication exists specifically for sleep disorders in children. Here are five medications commonly used to address sleep issues in children with autism:
- Melatonin: A natural hormone that regulates sleep-wake cycles. Available over-the-counter, it helps with falling asleep and staying asleep. Side effects include headaches, dizziness, and morning grogginess.
- Clonidine: A prescription medication originally for high blood pressure. It helps with sleep initiation and reduces night awakenings. Potential side effects include drowsiness and low blood pressure.
- Guanfacine: Another prescription drug for managing ADHD symptoms, it can also aid in sleep. Side effects may include sedation, dizziness, and weight gain.
- Diphenhydramine (Benadryl): An over-the-counter antihistamine that induces drowsiness. It’s not recommended for long-term use due to side effects like hyperactivity in some children and reduced effectiveness over time.
- Risperidone & Clonazepam: Reserved for severe cases, these prescription medications address behavioral issues and sleep but come with significant risks, including weight gain and dependency.
Each child reacts differently to medications, so working closely with a healthcare provider is essential for safe and effective treatment. Tracking sleep patterns and side effects with tools like the Guiding Growth app can help optimize care.
Insomnia Medication Guidelines for Children in the Context of ASD & ID (Daniel Castellanos, MD)
1. Melatonin
Melatonin is a hormone naturally produced in the brain, playing a key role in regulating the sleep-wake cycle in children. However, many autistic children face challenges with their internal clock. Research suggests that about 65% of children with autism spectrum disorder (ASD) have lower melatonin levels.
Uses
Melatonin supplements are often used to help children who have trouble falling asleep or staying asleep. This hormone promotes sleepiness, making it easier for children to settle down at night. There are two primary forms of melatonin supplements:
- Immediate-release melatonin: Helps children fall asleep more quickly.
- Prolonged-release melatonin: Assists in maintaining sleep throughout the night.
Benefits
Research highlights the effectiveness of melatonin in improving sleep for children with ASD. For instance, immediate-release melatonin has been shown to increase total sleep duration by approximately 73 minutes and reduce the time it takes to fall asleep by 66 minutes. Combining 3 mg of melatonin with cognitive-behavioral therapy has resulted in significant improvements for over 60% of children.
While these benefits are encouraging, it’s important to monitor usage closely due to possible side effects.
Potential Side Effects
Although melatonin is generally well-tolerated, it can cause some side effects. Common issues include fatigue, headaches, dizziness, mood changes, stomach discomfort, morning grogginess, vomiting, and upper respiratory infections. Less frequent side effects may include bedwetting, night terrors, nightmares, or other sleep disturbances. Additionally, melatonin can interact with medications such as blood thinners and antidepressants, so caution is needed.
One noteworthy concern is that over 70% of melatonin supplements might not contain the exact amount listed on their labels, raising questions about consistency and reliability.
Prescription Status
Melatonin is available over-the-counter as a dietary supplement. However, unlike prescription medications, it is not regulated by the FDA. Its use for sleep issues in autistic children is considered off-label. Despite its accessibility, experts strongly advise consulting a pediatrician before starting melatonin. This ensures the correct dosage, timing, and monitoring for any possible interactions or side effects.
2. Clonidine
Clonidine is a prescription medication originally developed to manage high blood pressure but is also used off-label to address sleep disturbances in children with autism. Unlike melatonin, which regulates the sleep-wake cycle, clonidine works directly on the central nervous system to promote sleep.
Uses
Clonidine is especially helpful for children who have difficulty falling asleep at bedtime, a condition known as sleep initiation trouble. Research indicates that 86.1% of children prescribed clonidine for sleep disturbances struggled specifically with sleep onset issues. It can also help reduce night awakenings, making it a versatile option for improving sleep quality.
In addition to its effects on sleep, clonidine may provide secondary benefits such as reducing hyperactivity, improving attention, stabilizing mood, and easing aggressive behaviors. However, its primary role remains focused on addressing sleep-related challenges.
Benefits
Studies have highlighted clonidine’s ability to significantly shorten the time it takes for children with autism to fall asleep and reduce the frequency of night awakenings. Some research also points to improvements in irritability and other related behaviors.
Potential Side Effects
While clonidine can be effective, it’s essential to consider its potential side effects. Common issues include drowsiness, dry mouth, dizziness, headaches, nausea, tiredness, weakness, constipation, and blurred vision. A study on extended-release clonidine in children and adolescents found that 65.5% of participants experienced adverse effects, with drowsiness being the most frequently reported.
More serious but less common side effects can include irregular or slow heartbeat, confusion, and severe gastrointestinal problems. Parents should monitor for dizziness or lightheadedness, especially when their child stands up quickly. It’s also worth noting that clonidine can amplify the effects of alcohol and other central nervous system depressants.
Prescription Status
Clonidine is available only with a prescription and requires careful dosage adjustments under the supervision of a healthcare provider. Abruptly stopping the medication is not recommended, as it can cause dangerous spikes in blood pressure. Instead, healthcare providers typically advise tapering the dose gradually to safely discontinue use.
3. Guanfacine
Guanfacine, initially developed to treat high blood pressure, is often prescribed off-label to help manage behavioral issues and sleep problems in children with autism. This medication provides a unique combination of benefits: it not only helps with attention and anxiety but also supports easier sleep onset and a more consistent sleep routine.
Uses
Guanfacine is commonly used to address symptoms like inattention, hyperactivity, and impulsivity in children with autism spectrum disorder (ASD). When it comes to sleep, guanfacine can help children fall asleep more easily and maintain a regular sleep schedule. Additionally, it may reduce anxiety levels that often disrupt sleep. Clinical studies back these uses, showing noticeable improvements in both behavior and sleep patterns.
Benefits
Research highlights guanfacine’s effectiveness for children with autism. In a multicenter randomized study involving 62 children with ASD, those who took extended-release guanfacine experienced significant improvements compared to those on a placebo. About 50% of the guanfacine group showed marked progress, compared to just 9.4% of the placebo group. Interestingly, nearly half of the children who didn’t respond to methylphenidate saw significant benefits when switched to guanfacine.
Potential Side Effects
While guanfacine offers several advantages, it can also cause side effects. Common issues include sedation, dizziness, headaches, nausea, stomach pain, constipation, dry mouth, sleepiness, and weight gain. More serious side effects might include low blood pressure (hypotension), a slow heart rate (bradycardia), and fainting (syncope). Parents should watch for warning signs like blurred vision, confusion, severe dizziness, chest pain, difficulty breathing, irregular heartbeat, or extreme fatigue.
Prescription Status
Guanfacine is a prescription-only medication. Careful dose adjustments and regular monitoring of blood pressure and heart rate are crucial. It’s also important for parents to consult with their healthcare provider before combining guanfacine with other medications, including over-the-counter drugs or herbal supplements.
4. Diphenhydramine (Benadryl) and Other Antihistamines
Diphenhydramine, commonly known as Benadryl, is an antihistamine originally designed to treat allergies. However, its sedative side effect has led to its off-label use as a sleep aid, including for autistic children. While it may seem like a convenient option, its use in this context requires careful consideration.
Uses
Antihistamines like diphenhydramine are sometimes used to promote drowsiness due to their ability to block H1-histamine receptors in the brain, which results in sedation. In fact, a survey by the American Academy of Pediatrics identified antihistamines as the most frequently reported nonprescription option for sleep issues.
However, experts emphasize that antihistamines should not be the first choice for addressing sleep disturbances in children with neurodevelopmental conditions. The lack of controlled trials and concerns about tolerability raise red flags. Many specialists advocate starting with behavioral strategies and good sleep hygiene before turning to medications. This approach helps balance the quick-acting nature of diphenhydramine against its potential downsides.
Benefits
One of the main advantages of diphenhydramine is its easy availability over the counter. It also works relatively quickly to induce sleep. That said, the benefits may diminish over time as the body builds tolerance, reducing its effectiveness with prolonged use.
Potential Side Effects
While diphenhydramine can help induce sleep, it comes with a range of side effects. Common issues include drowsiness, dry mouth, dizziness, and trouble focusing. Interestingly, about 10–15% of children may experience the opposite effect – hyperactivity, making it counterproductive as a sedative. Others might encounter excitability or agitation instead of the expected calming effect.
More serious side effects can include irregular heartbeat, numbness, restlessness, and confusion. In rare cases, it can lead to seizures, severe allergic reactions, or urinary retention. These risks highlight the importance of careful monitoring.
Prescription Status
Diphenhydramine is available in various over-the-counter forms, including tablets, capsules, liquids, and topical applications. It’s crucial to follow the label instructions carefully. Over-the-counter products are approved only for children aged 6 and older, with specific maximum daily doses. For children aged 6 to 12, the limit is 150 mg per day, while individuals over 12 can take up to 300 mg daily.
Important safety tips include avoiding antihistamines for children under 4, not doubling doses, and never combining two different antihistamines unless directed by a healthcare provider. Additionally, children and people over 65 are more sensitive to antihistamines and should use them with extra caution. As with any medication, proper dosing and close monitoring are key to ensuring safe use.
sbb-itb-d549f5b
5. Risperidone and Clonazepam
Risperidone and clonazepam are typically considered when first-line treatments fail, especially for older children or teenagers with autism who struggle with sleep and behavioral challenges. These medications are less commonly used but may be helpful in specific cases where standard options are insufficient.
Uses
Risperidone, an antipsychotic, is often prescribed to address mood and behavioral issues. An added benefit is that it may help improve sleep quality. Clonazepam, a benzodiazepine mainly prescribed for seizures and anxiety, is sometimes used off-label to aid sleep when other treatments are ineffective.
Benefits
For children who don’t respond to first-line treatments, these medications may offer some relief. Risperidone can help manage behavioral problems and may indirectly support better sleep. Clonazepam, while primarily used for other conditions, has shown to provide satisfaction in certain cases where sleep issues are severe. However, the potential benefits must always be carefully weighed against the risks.
Potential Side Effects
Risperidone is associated with a range of side effects, including significant weight gain (about 6 pounds in just eight weeks), increased appetite, drowsiness, metabolic problems, and risks of tardive dyskinesia and hyperprolactinemia. Studies have reported adverse effects in up to 77% of patients treated with risperidone.
This rise in prolactin can result in breast development in boys, lactation in girls, menstrual irregularities, and even sexual dysfunction. Other serious risks include hyperglycemia, high cholesterol, orthostatic hypotension, seizures, and, though rare, neuroleptic malignant syndrome.
Clonazepam carries its own risks, including dependency and excessive sedation. Long-term use can make discontinuation particularly challenging.
Prescription Status
Due to the potential for serious side effects, both risperidone and clonazepam require careful consideration and close monitoring by healthcare professionals. These medications are prescription-only and should only be used under the guidance of a specialist, such as a pediatric psychiatrist or developmental pediatrician, who is experienced in managing autism-related sleep and behavioral issues. Their use is typically reserved for cases where other interventions have not been successful, and ongoing medical supervision is essential.
How to Track Sleep and Medication Effects with Guiding Growth
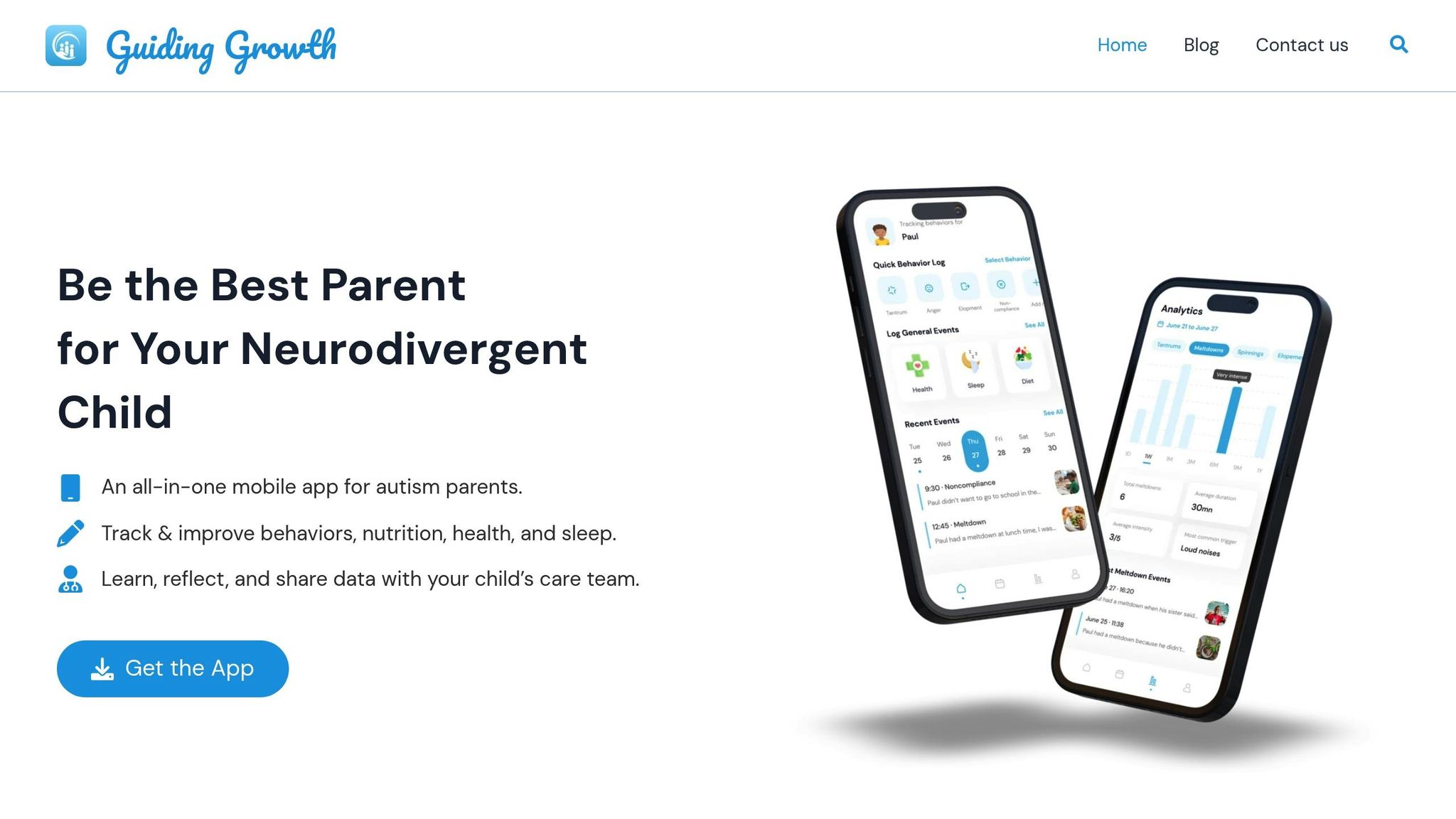
Effectively tracking your child’s sleep and medication can make a world of difference. With about 44–83% of children on the autism spectrum facing sleep challenges, having a clear record of what works and what doesn’t is essential. Guiding Growth simplifies this process, helping you monitor medication and sleep patterns in one convenient place, while also providing valuable insights for healthcare discussions.
All-in-One Sleep and Medication Tracking
Guiding Growth brings everything together (sleep patterns, medication schedules, and potential side effects) all in one app. From bedtime routines to medication timing, every detail can be logged for accurate analysis.
Simplified Medication Management
Medication tracking is just as important as monitoring sleep. Guiding Growth excels at combining medication records with therapy and healthcare visit logs, offering a clear view of behavioral trends over time. This allows you to document changes in appetite, mood, or sleep that could signal the need for treatment adjustments.
Spotting Triggers and Patterns
The app goes beyond basic tracking by helping parents identify triggers. By logging specific behaviors, events, or environmental changes, you can uncover how these factors affect your child’s sleep and overall well-being. Over time, this data empowers you to make more informed decisions about treatment and daily routines.
Streamlined Communication with Professionals
One of the standout features of Guiding Growth is its ability to generate clear, easy-to-read reports. These reports can be shared with doctors and therapists, providing a detailed overview of your child’s progress and challenges. Instead of relying on memory during appointments, you’ll have comprehensive data to guide discussions about dosage adjustments or medication changes. This is especially helpful for treatments that require close monitoring.
Medication Comparison Table
When deciding on a medication for your child’s sleep challenges, it’s important to weigh the purpose, benefits, and potential side effects of each option.
| Medication | Prescription Status | Primary Uses | Key Benefits | Common Side Effects | Special Considerations |
|---|---|---|---|---|---|
| Melatonin | Over-the-counter | Helps children fall asleep | Natural supplement; generally well-tolerated; non-habit forming | Nausea, headache, dizziness, hypothermia | Best for sleep initiation, not maintenance; timing is key |
| Clonidine | Prescription required | Induces sleepiness, reduces nighttime waking | Helps with both falling asleep and staying asleep | Hypotension, bradycardia, irritability, dry mouth, reduced REM sleep | Must discontinue gradually to avoid rebound hypertension |
| Guanfacine | Prescription required | Sleep support and ADHD management | Can aid in sleep regulation | Hypotension, bradycardia, irritability, dry mouth, reduced REM sleep | Often prescribed off-label; regular blood pressure monitoring needed |
| Diphenhydramine (Benadryl) and Other Antihistamines | Over-the-counter | Sleep induction via antihistamine effects | Easily accessible with sedative properties | Sedation, fever, blurred vision, dry mouth, constipation, confusion | May cause lingering drowsiness the next day |
| Risperidone & Clonazepam | Prescription required | Used for severe cases when other treatments fail | Effective for significant sleep and behavioral issues | Risperidone: Weight gain, diabetes risk, prolactin elevation Clonazepam: Dependence, cognitive issues, rebound insomnia | Reserved for older children/teens; requires close medical oversight |
Melatonin remains one of the most accessible options, available over-the-counter in various strengths across the United States and Canada. According to a community survey, about 15% of pediatricians have recommended melatonin for children experiencing sleep issues. Similarly, antihistamines like diphenhydramine are a frequent non-prescription choice, often suggested by pediatricians for their sedative effects.
Age plays a significant role in deciding on medication. Stronger options like risperidone and clonazepam are typically reserved for older children and teenagers when other treatments have failed. These medications require careful monitoring due to their potential for dependency and serious side effects.
It’s always best to start with the lowest effective dose and adjust gradually, keeping a close eye on any side effects. Use this table as a guide when discussing options with your child’s healthcare provider.
Conclusion
Choosing the right sleep medication for your autistic child can feel like navigating uncharted waters. It requires patience, collaboration with your healthcare team, and close observation of how your child responds to treatment. Each medication has its own purpose, along with specific benefits and potential risks.
Since autism spectrum disorder presents differently in every individual, a tailored approach is key. This becomes even more crucial when considering that about 70% of autistic individuals experience at least one other physical or mental health condition, such as anxiety, epilepsy, or ADHD.
Starting with gentler options, like over-the-counter melatonin, is often a good first step. For more complex sleep challenges, prescription medications might be necessary, with stronger treatments reserved for cases where other approaches haven’t worked. These decisions should always be made in consultation with your healthcare provider to ensure the best possible outcome.
Tracking your child’s sleep patterns and medication effects can make a huge difference in managing their care. Tools like Guiding Growth can help you record details like sleep quality, timing, side effects, and behavioral changes, turning daily observations into actionable insights. This information can help you have more productive discussions with your child’s doctor and fine-tune their treatment plan.
FAQs
How can I find the best medication to help my autistic child with sleep problems?
When addressing your autistic child’s sleep difficulties, the first step is to consult a healthcare professional. They will evaluate your child’s individual needs, medical history, and any factors that might be influencing their sleep patterns. One common recommendation is melatonin, which can assist in regulating sleep-wake cycles for autistic children. However, depending on your child’s circumstances, other medications might be more suitable.
It’s crucial to follow your doctor’s instructions regarding the type of medication and the proper dosage to ensure both safety and effectiveness. Maintaining open and ongoing communication with your child’s healthcare provider is essential for identifying the best approach tailored to their needs.
What should I know before giving my child melatonin for sleep issues?
Before considering melatonin for your child, it’s crucial to talk to a healthcare provider. They can confirm whether it’s suitable and help you find the right dosage. Using melatonin incorrectly or too often can cause side effects like drowsiness, irritability, or an upset stomach. Stick to medical advice and keep an eye on how your child responds.
Store melatonin safely out of your child’s reach to avoid accidental ingestion, and only use it as directed. Keep in mind, melatonin is meant to support sleep, not replace good sleep habits or a consistent bedtime routine.
What’s the best way to track my child’s response to sleep medications and ensure they’re safe?
To effectively monitor your child’s response to sleep medications and ensure their safety, it’s important to keep a detailed daily record. Track their sleep habits, any changes in mood or behavior, and watch for potential side effects such as unusual actions or physical symptoms. Documenting these observations can help identify patterns and detect any concerns early.
Consider using the Guiding Growth app to simplify this process. The app allows you to log sleep patterns, behaviors, and symptoms in one place, making it easier to share accurate, organized information with your child’s healthcare provider. Regular updates can help the provider evaluate how well the medication is working and whether any adjustments are needed. If you notice anything worrisome, don’t hesitate to contact the doctor right away.


